

Splitting the patients by low versus normal AMTS showed that MoCA scores were significantly lower in patients with AMTS <8 versus ≥8 (mean/SD MoCA = 11.3/4.9 vs. Ethics approval was subsequently granted for inclusion in the Oxford Cognitive Comorbidity, Frailty and Ageing Research Database (ORCHARD REC reference 18/SC/0184).ĩ6/205 (46.8%) had low AMTS, and 174/185 (94%) testable patients had cognitive impairment on the MoCA overall: 74 (40%) had mild (MoCA <26, ≥18) and 100 (54%) had moderate/severe impairment (MoCA <18) with the remaining 11 being unimpaired (Table 1, Fig.
#MOCA COGNITIVE ASSESSMENT VERSUS OTHER TESTS REGISTRATION#
The study was registered with the Oxford University Hospitals Audit Team (audit registration No. The study was undertaken to inform future service development as part of a programme to improve the process of care for patients with comorbid cognitive disorders and was approved by the Divisional Management. Some data on the 2013 cohort have been reported previously.
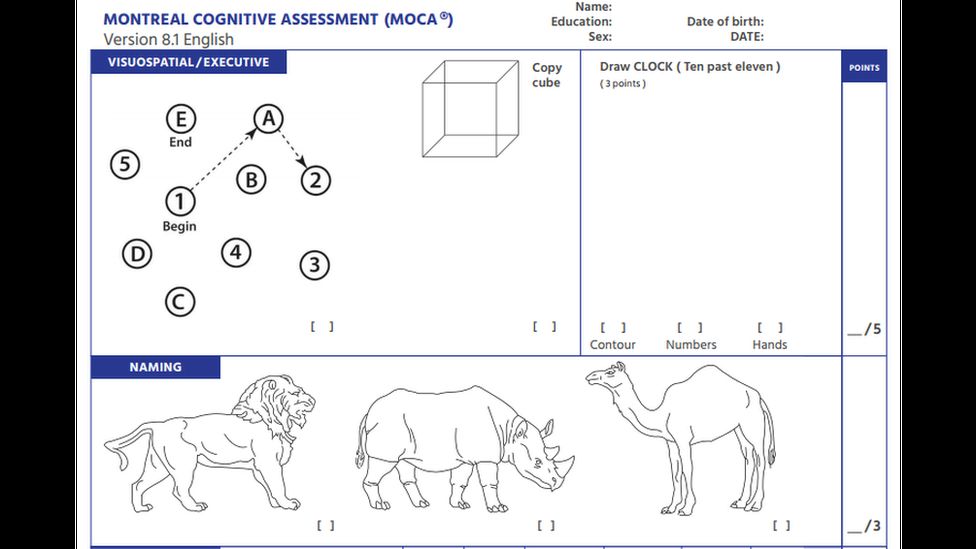
Patients were eligible if aged ≥75 years, able to participate in testing and were not receiving end of life care. In a prospective observational study, consecutive patients staying at least ≥72 h on a medical ward from March to May 2013 and from March to July 2017 were examined. The Oxford University Hospitals Trust provides services for all acute internal medicine patients in a population of approximately 660,000 and runs an unselected medical admission system irrespective of age. The AMTS cannot therefore be used as a “rule-out” test, and more detailed cognitive assessment will be required in selected patients. Conclusion: The AMTS is highly specific but relatively insensitive for cognitive impairment: a quarter of those with normal AMTS had moderate/severe impairment on the MoCA with widespread deficits. All MoCA subtests discriminated between low and normal AMTS groups (all p < 0.0001, except p = 0.002 for repetition) but deficits in delayed recall, verbal fluency and visuo-executive function were prevalent even in the normal AMTS group. The negative predictive value of AMTS <8 was therefore low for mild impairment (10.9%, 5.6–18.7) but much higher for moderate/severe impairment (75.2%, 65.7–83.3). AUC of the AMTS for mild and moderate/severe impairment were 0.86 (95% CI = 0.80–0.93) and 0.88 (0.82–0.93), respectively. Moderate/severe cognitive impairment was more prevalent in the low versus the normal AMTS group: 74/83 (90%) versus 25/102 (25%, p < 0.0001). Sensitivity, specificity, positive and negative predictive values of low AMTS (<8) for cognitive impairment were determined. Reliability of the AMTS for the reference standard defined as mild (MoCA <26) or moderate/severe (MoCA <18) cognitive impairment was assessed using the area under the receiver-operating curve (AUC). Methods: The AMTS and MoCA were administered to consecutive hospitalized patients at ≥72 h after admission in a prospective observational study. We therefore studied the AMTS versus the 30-point Montreal Cognitive Assessment (MoCA) in older (≥75 years) inpatients. The 10-point Abbreviated Mental Test Score (AMTS) is widely used in acute hospital settings but its reliability for mild versus more severe cognitive impairment is unknown.

Screening to identify cognitive deficits is therefore important to optimize care. Background/Aims: Cognitive impairment is prevalent in older inpatients but may be unrecognized.


 0 kommentar(er)
0 kommentar(er)
